Health care's move to outcomes and value is transforming the industry, and payers are leading the charge. This makes payers an increasingly influential customer for pharma. Yet navigating the complex and fragmented payer landscape at a time when health care is dramatically changing—both in how it is delivered and in how it is paid for—has been challenging for pharma and raised many questions about what payers want, their attitudes and how best to engage with them.
To address some of these questions, we recently surveyed 30 US payers, 30 European payers and 18 pharmaceutical company representatives from functions such as market access and managed markets. We asked payers about their business challenges and attitudes as well as the kind of trial data they regarded as most important. Then, to determine how well pharma companies understood payers' needs and attitudes, we asked pharma companies to identify payers' needs and attitudes and compared their answers to those provided by payers.
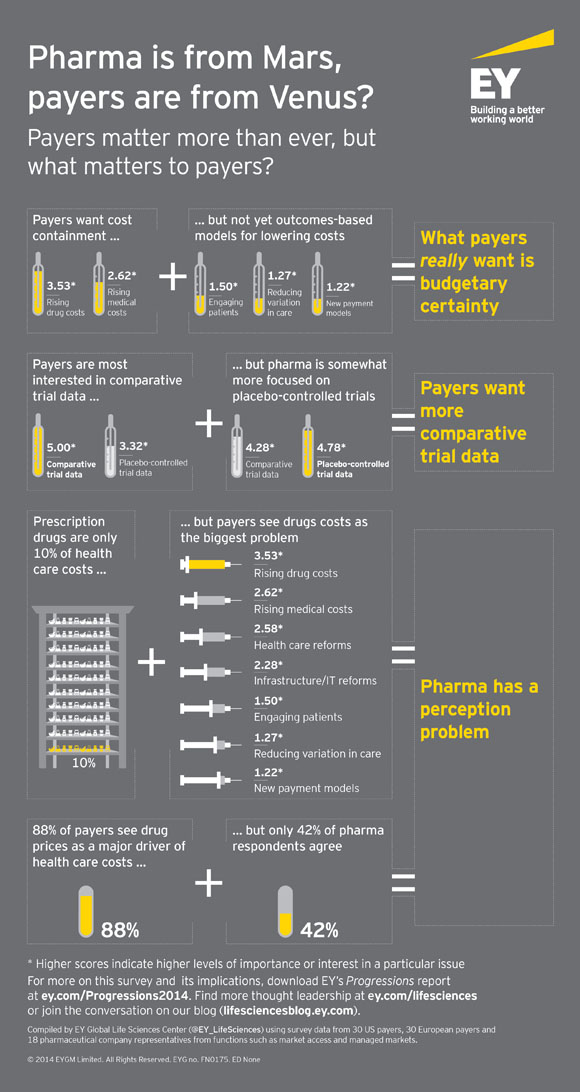
The survey revealed differences across payers and markets but also some common threads:
- Payers want cost containment over outcomes-based approaches to containing costs. The results showed a striking gap between their high focus on costs and their relatively low interest in the outcomes-based approaches that are widely regarded as the most sustainable way to bring costs under control. The top two business challenges payers cited were "curbing rising drug costs" and "curbing rising medical (non-drug) costs," while value- and outcomes-based initiatives such as "engaging patients," reducing variation in care" and "contracting with providers via new payment models" were ranked at the bottom.
- Pharma is not moving quickly enough on comparative trials. While pharma companies are generally well aligned with payers' data needs, one area of disconnect is clinical trial data, which payers still regard as the gold standard. Payers are most interested in comparative trial data (e.g., head-to-head trials versus standard of care), which best measure the differential value of a new product. But, while payers rank comparative trial data as their most important data type, pharma companies report that the data they use most for demonstrating value is instead placebo-controlled
- Pharma has a perception problem. Even though prescription drugs are only about 10% of health care spending, payers see drug costs as their biggest challenge. While pharma companies' perception of payers' strategic priorities is pretty well aligned with payers' thinking, pharma companies tend to underestimate the importance given to drug costs and overestimate the significance of non-drug costs. In addition, when we asked payers whether they agreed with certain statements about the pharmaceutical industry, the statement they most emphatically agreed with was "drug prices are a major driver of health care cost increases"—88% of payers strongly or somewhat agreed. Meanwhile, only 42% of pharma respondents strongly or somewhat agreed with this statement.
This perception problem will become increasingly relevant at a time when pharma companies will need to engage with payers in new ways. We plan to discuss this trust gap—and what pharma can do about it — in an upcoming blog post.
For more on our survey and our 2014 report on the pharmaceutical industry, Progressions—navigating the payer landscape, go to www.ey.com/Progressions2014.
Patrick Flochel
EY